Can Antibodies Be Used to Treat Covid-19?
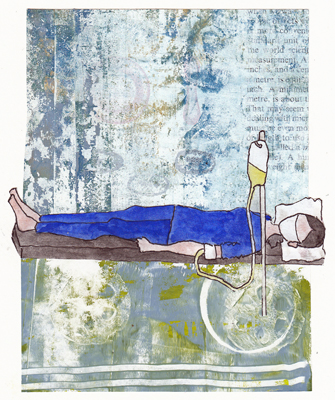
When you transfuse antibodies into patients, you develop "passive, instead of natural immunity." During the 1918 flu pandemic, patients who recovered from influenza donated blood so their antibodies could be transfused into other critically ill patients. More recently, "convalescent plasma" from recovered Ebola patients was given to other patients. Randomized control trials (RCT) are being done to test "convalescent plasma" for Covid-19 patients, but in addition MONOCLONAL ANTIBODIES are being developed from blood obtained from recovered patients. Read about them below the collage.
Patients who have recovered from Covid-19 have naturally occurring immunity against all parts of the SARS-CoV-2 virus. Their antibodies and immune cells are being studied, and the strongest neutralizing antibodies (which stop viral replication), are used to develop monoclonal antibodies which can be produced in large quantities. This technology was first developed in the 1970s and is now being used to create many types of therapy, including cancer drugs. In the classic method, cells which are producing antibodies are fused with a specific clone of antibody producing cells that can be grown in culture. This clone becomes a protein factory which makes just one potent neutralizing antibody. There are many monoclonal antibodies being made to SARS-CoV-19 and at least 3 are in early clinical trials. Passive immunity with monoclonal antibodies is only effective for weeks to a month+, but when administered they can change the course of critically ill patients. You can usually recognize monoclonal antibodies that are FDA approved because their names end with "ab."